Information 1-3
- Undertaken to identify, manage and prevent ear disease and hearing loss
Health check recommendations
- All adults > 15 years of age if clinically indicated
- All Aboriginal and Torres Strait Islander > 15 years of age annually
1. Procedure
- Ask the questions and perform the corresponding procedure. See Table 1.
- Provide brief intervention as required
- Determine if the person requires a referral and place on a follow-up and recall register. See Flowchart 1.
Table 1. Questions and procedures for adult ears and hearing | |
|---|---|
Questions | Explore |
Do you have any difficulty hearing? |
|
Do you have any ear pain or discharge? | |
- Performing otoscopy 1–3
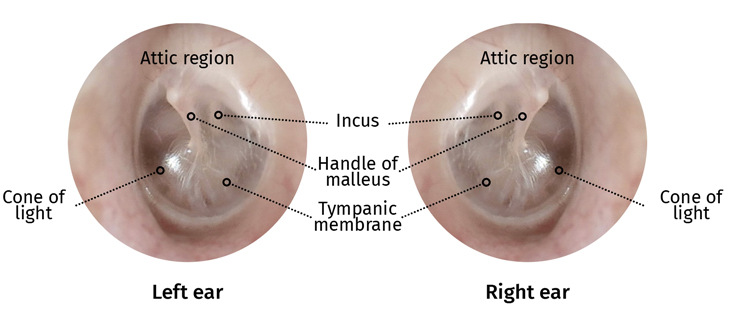
- Otoscopy is the visual examination of the ear canal and eardrum. See Figure 1.
- If there is pain or notable discharge from the ear(s) do not proceed. Refer to the Primary Clinical Care Manual
- Observe the bone behind the ear (mastoid) and the area under the ear for infection, swelling or tenderness
- Check the pinna for size, shape, colour or lesions
- Observe the ear canal for:
- discharge
- redness/swelling
- fungal infections
- lumps or bony growths
- foreign bodies
- wax
- fluid
- Inspect the eardrum (tympanic membrane) for:
- colour:
- transparent and shiny is normal
- dull or opaque represents fluid behind eardrum
- cone of light (reflection):
- right ear at 5 o’clock and left ear at 7 o’clock
- reflections elsewhere indicates bulging
- the handle of the malleus
- perforations
- abnormalities of the attic region e.g. perforation, mass, growth
- colour:
- Repeat procedure for the other ear
Figure 1. Visual representation of the eardrums
Flowchart 1. Hearing health check review and referral procedure

- Performing tympanometry 1–3
- Tympanometry is a test of middle ear function and measures:
- ear canal volume (ECV)
- middle ear pressure (daPa)
- middle ear compliance or movement
- See Resource 1. for further tympanometry support
- If a person has had recent surgery, pain or if there is a perforation or discharge from the ear(s) do not proceed. Refer to the Primary Clinical Care Manual
- A “Leak” or “Blockage” error can occur for many reasons:
- clogged probe tip
- probe tip too large or small
- head movements or swallowing
- probe tip against the ear canal wall
- debris, foreign body or wax in ear canal
- To rectify try:
- a different sized probe tip
- cleaning probe tip
- reposition the probe tip in the ear canal
- Tympanometry is a test of middle ear function and measures:
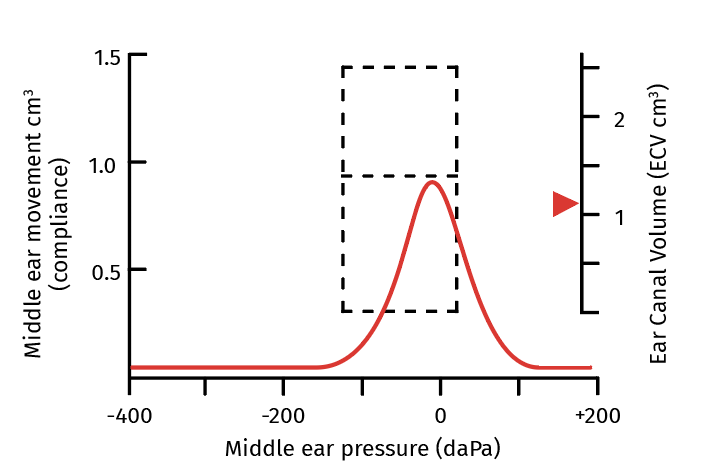
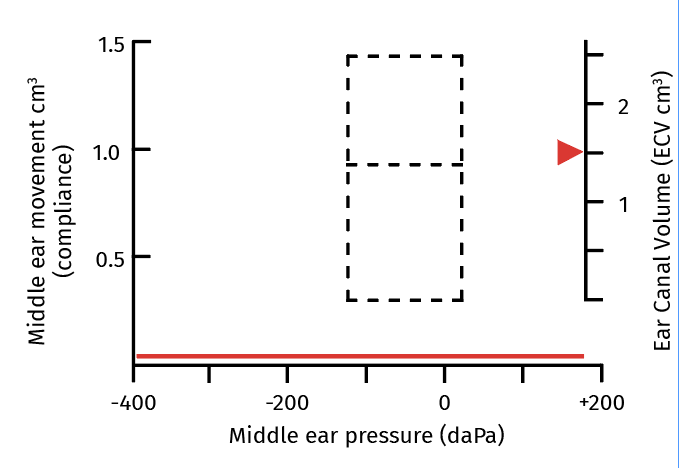
Figure 2. Tympanometry traces 1–3
Type A Normal
|
|
Type B Fail
Possible causes
|
|
Type C Fail
Possible causes
|
|
- Performing audiometry 1–3
- Audiometry measures the ability of the ear to:
- detect the pitch of a sound as hertz (Hz)
- detect the loudness of a sound as decibels (dB)
- Place headphones on patient. Test one ear at a time
- Set hertz (Hz) dial to 4000 Hz and decibels (dB) to 50 dB. Test
- The person ‘fails’ if they do not indicate they hear a sound
- If the person indicates they can hear the sound then reduce to 35 dB and repeat
- If the person indicates they can hear the sound then reduce to 25 dB and repeat
- Repeat these steps until the person no longer responds
- Record the lowest perceived dB the person responds to twice
- Repeat for the other ear
- Repeat the procedure for both ears at 2000 Hz and 1000 Hz
- To ‘pass’, the person needs to respond twice to 25 dB at 1000, 2000 and 4000 Hz
- Audiometry measures the ability of the ear to:
2. Results
- All adults should have
- clean ears, free of pain, discharge or infection
- pass all tests and hear clearly
3. Brief intervention 1–3
- Ear disease and hearing loss is high in Aboriginal and Torres Strait Islander adults, related to frequent childhood ear infections, contributing to poor education, unemployment and justice system contact
- Provide preventative information:
- hand and face washing
- regular nose blowing
- avoid cigarette/vape smoke
- avoid loud noises (e.g. earbuds or headphones)
- only swim in running water or swimming pools
- maintain healthy Diet and nutrition
- avoid putting anything in the ears (including cotton buds)
- if concerned present to health centre
4. Referral
- If you have any concerns about a person’s ability to hear refer to MO/NP and email Hearing Australia. See Resource 2–3.
- If the person has ear pain or discharge, manage according the Primary Clinical Care Manual
5. Follow-up
- Review as per Flowchart 1.
- Place the person on a recall register if required
- Ensure all referrals are actioned
- Provide the person with details for the next scheduled follow-up appointment
6. References
- All Chronic Conditions Manual references are available via the downloadable References PDF