Information 1–4
- Undertaken to identify and monitor ear diseases that can cause long term hearing loss affecting a child’s:
- speech and language
- ability to play and develop socially and emotionally
- ability to learn and have positive educational outcomes
- see Developmental milestones
Note
- Refer to the Primary Clinical Care Manual to manage acute ear presentations
Health check recommendations
- All children have a hearing screen at birth
- All children if clinically indicated opportunistically
- Aboriginal and Torres Strait Islander children < 6 years at each scheduled health check or opportunistically
- Aboriginal and Torres Strait Islander children > 6 years annually
1. Procedure
- Ask child or parent the age appropriate questions, explore any concerns and take the corresponding actions. See Table 1.
- Provide brief intervention
- Determine if the child requires a referral according to the criteria and place on a follow-up and recall register. See Flowchart 1.
Table 1. Questions and actions for child ears and hearing | ||
|---|---|---|
Age | Questions | Action |
1–6 weeks |
|
|
2–12 months |
|
|
18 months to 5 years |
|
|
All Aboriginal and Torres Strait Islander children and children living in rural and remote locations:
All non-Aboriginal and Torres Strait Islander children
|
| |
> 5 years |
|
|
Flowchart 1. Hearing health tests and referral procedure
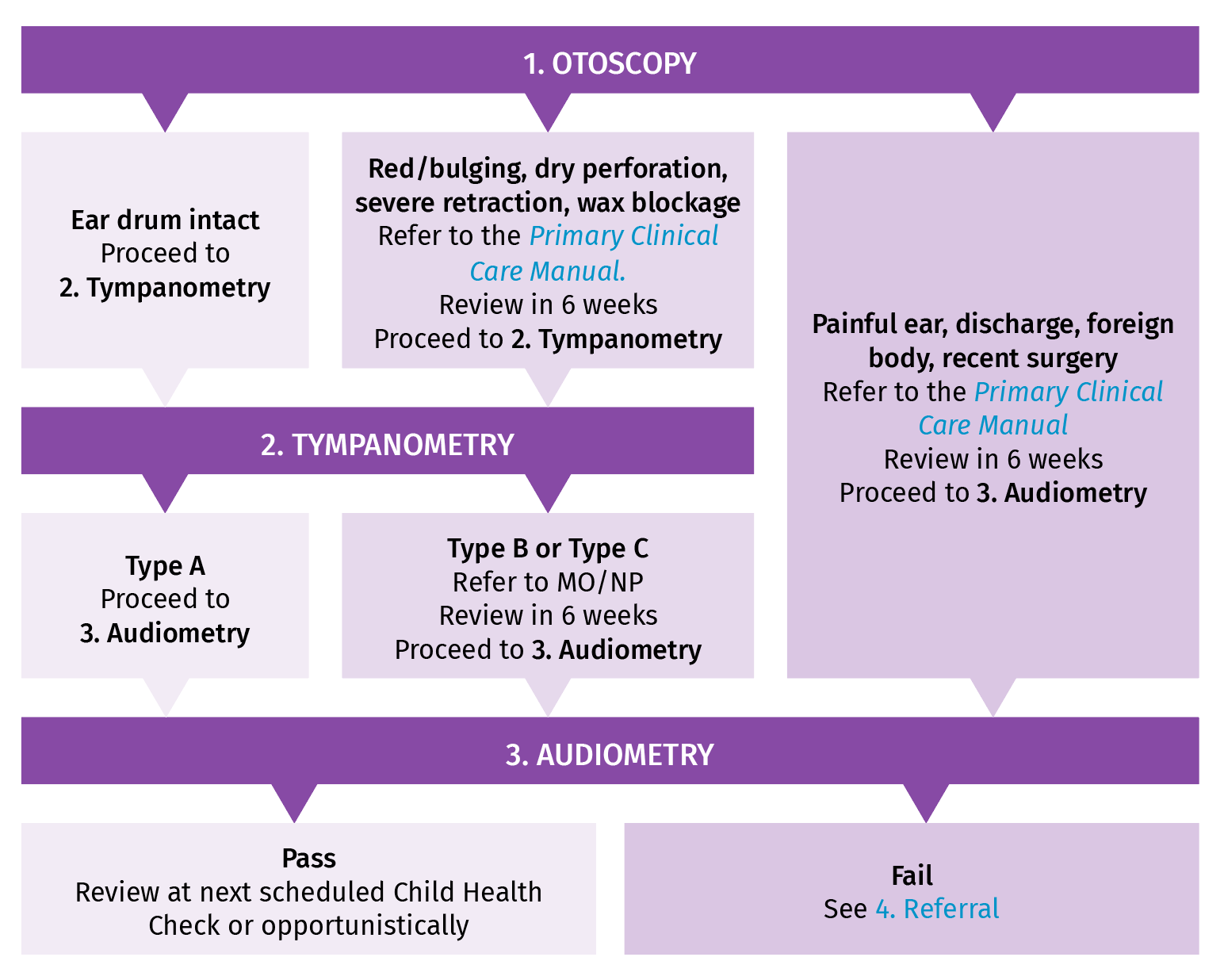
- Performing otoscopy 1–3
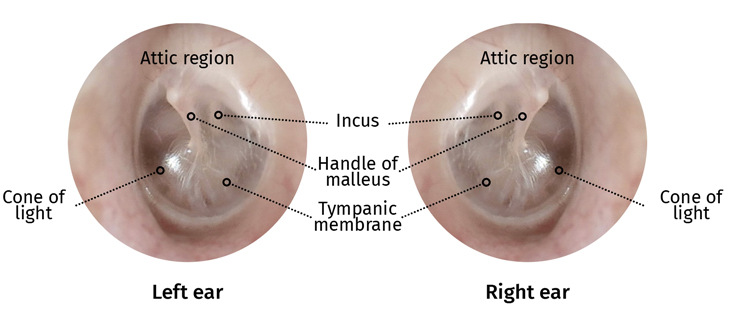
- Otoscopy is the visual examination of the ear canal and ear drum. See Figure 1.
- If there is pain or notable discharge from the ear(s) do not proceed. Refer to the Primary Clinical Care Manual
- Observe the bone behind the ear (mastoid) and the area under the ear for
infection, swelling or tenderness - Check the pinna for size, shape, colour or lesions
- Observe the ear canal for:
- discharge
- redness/swelling
- fungal infections
- lumps or bony growths
- foreign bodies (excluding grommets)
- wax
- fluid
- Inspect the eardrum (tympanic membrane) for:
- colour:
- transparent and shiny is normal
- dull or opaque represents fluid behind the eardrum
- cone of light (reflection):
- right ear at 5 o’clock and left ear at 7 o’clock
- reflections elsewhere indicates bulging
- the handle of the malleus
- perforations
- abnormalities of the attic region e.g. perforation, mass, growth
- colour:
- Repeat procedure for the other ear
Figure 1. Visual representation of the eardrums
- Performing tympanometry 1–3
- Tympanometry is a test of middle ear function and measures:
- ear canal volume (ECV)
- middle ear pressure (daPa)
- middle ear compliance or movement
- See Resource 1. for further tympanometry support
- If there is discharge from the ear(s) do not proceed. Refer to the Primary Clinical Care Manual
- A “Leak” or “Blockage” error can occur for many reasons:
- clogged probe tip
- probe tip too large or small
- head movements or swallowing
- probe tip against the ear canal wall
- debris, foreign body or wax in ear canal
- To rectify try:
- a different sized probe tip
- cleaning probe tip
- reposition the probe tip in the ear canal
- Tympanometry is a test of middle ear function and measures:
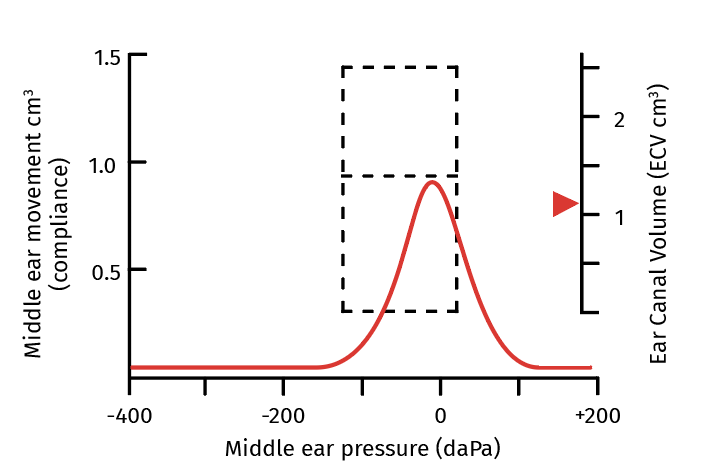
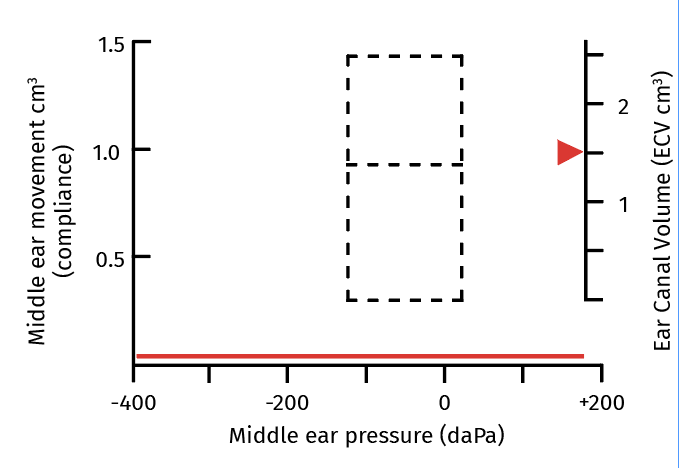
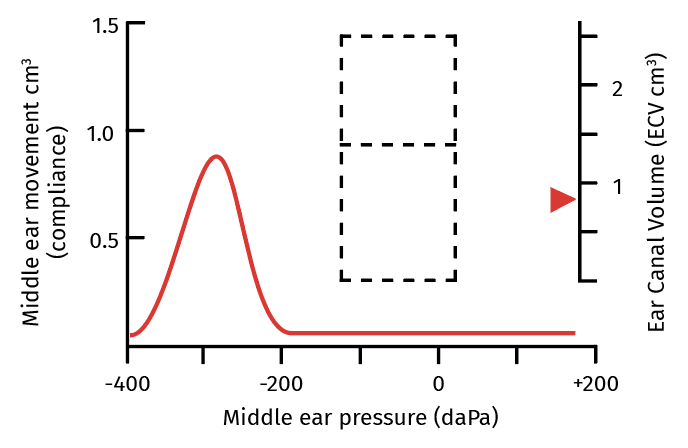
Figure 2. Tympanometry traces 1–4
Type A Normal
|
|
Type B Fail
Possible causes
|
|
Type C Fail
Possible causes
|
|
- Performing audiometry 1–4
- Audiometry measures the ability of the ear to:
- detect the pitch of a sound as hertz (Hz)
- detect the loudness of a sound as decibels (dB)
- For younger children:
- place the headphones on the desk (not child) and set to 4000 Hz and 90 dB
- present the tone and encourage them to clap, press button etc. if sound heard
- praise their response
- change frequency to ensure they respond when the sound is slightly different
- once they are able to respond reliably, proceed with testing
- child ‘fails’ if they do not respond as expected
- Children will look for visual cues for when to respond. Ensure:
- child is positioned so they can’t see your hands, face or the audiometer
- tones are presented at irregular intervals to avoid child anticipating the sound
- Place headphones on the child. Test one ear at a time
- Set hertz (Hz) dial to 4000 Hz and decibels (dB) to 50 dB. Test
- The child ‘fails’ if they do not indicate they hear a sound
- If the child indicates they hear the sound then reduce to 35 dB and repeat
- If the child indicates they hear the sound then reduce to 25 dB and repeat
- Repeat these steps until the child no longer responds, then increase by 5 dB increments until they do
- Record the result that the child responds to twice at the lowest perceived dB
- Repeat for the other ear
- Repeat the procedure for both ears at 2000 Hz and 1000 Hz
- To ‘pass’, the child needs to respond twice to 25 dB at 1000, 2000, and 4000 Hz
- Audiometry measures the ability of the ear to:
2. Results
- All children should have
- clean ears, free of pain, discharge or infection
- pass all tests and hear clearly
3. Brief intervention 1–5
- Aboriginal and Torres Strait Islander children:
- experience the highest rates of middle ear disease and hearing loss in Australia
- develop ear issues earlier and more frequently and severely than the general population
- Educate parents that unresolved hearing loss creates challenges for children later in life, including:
- school completion rates
- health literacy levels
- vocational and job prospects
- social isolation
- mental health issues
- Discussion points:
- regular nose blowing
- hand and face washing
- avoid prop bottle feeding
- avoid bottle feeding a child to sleep
- avoid leaving bottles in a child’s cot
- avoid subjecting a child to smoke from cigarettes or camp fires
- only swim in running water or swimming pools
- maintain healthy Diet and nutrition
- avoid putting anything in child’s ears (including cotton buds)
- there are often no signs or symptoms of hearing loss
- if concerned, always present to the health centre
- avoid loud noises (e.g. headphones)
- Provide Resource 2.
4. Referral
- If the child has ear pain or discharge, refer to the Primary Clinical Care Manual
- Perform the PLUM and HATS screening questionnaires (Resource 3.) and email referral to Hearing Australia (Resource 4.) if:
- < 3½ and parent answers ‘no’ to screening questions
- the clinician is unable to undertake any hearing testing e.g. child too young, clinician is not experienced
- the child ‘fails’ audiometry or tympanometry for a second time after a 6 week review
- If clinician or the parent has any immediate concerns about a child’s hearing, refer to the MO/NP and speech pathologist
5. Follow-up
- Review as per Flowchart 1.
- Place the child on a recall register to monitor Developmental milestones, speech, hearing or ear disease if required
- Ensure all referrals are actioned
- Provide the parent with details for the next scheduled follow-up appointment
6. References
- All Chronic Conditions Manual references are available via the downloadable References PDF