Information 1–3
- Undertaken to monitor a child’s growth and act early on identified risks associated with growth and development or chronic conditions
- The World Health Organisation (WHO) standard growth charts are used from birth to 5 years. The Centre for Disease Control (CDC) Standard Child Growth charts can be used from 2 years of age. See Resource 1.
Health check recommendations
- All newborns at first 1–6 weeks postnatal visit
- Weight and length/height at each child health check to 5 years then:
- opportunistically until 15 years
- annually until 15 years for Aboriginal and Torres Strait Islander and rural and remote children
- Include a 9 month health check for Aboriginal and Torres Strait Islander and rural and remote children
- Head circumference at each child health check until 2 years
- Fontanelles palpated at 6, 12 and 18 months of age
- All children have body mass index (BMI) calculated once between 2½–3½ and 4–5 years, then opportunistically until 15 years of age
1. Procedure 1
- Perform the measurements as per Table 1.
- Plot the measurements on the appropriate chart e.g. length/height for age, weight for height or BMI for age. See Resource 1. and 2.
- Children born prematurely have their measurements plotted on a Fenton growth chart (Resource 3.) or according to their corrected age on a standard chart
Determining corrected age
Corrected age = baby’s age in weeks since birth minus the number of weeks premature (40 minus infants gestational age in weeks).Example:
A 16 week old infant born at 32 weeks
= 16 - (40 - 32)
= 16 - 8
= 8 weeks of age (corrected)
- < 37 weeks gestation have their age corrected for 1 year
- < 32 weeks gestation have their age corrected for 2 years
- Refer child to an appropriate clinician if anomalies are identified
- Provide brief intervention
- If a child requires follow-up assessment place on a recall register
Record all information in the child’s Personal Health Record booklet
Table 1. Body measurements for children | |
|---|---|
Measurement | Procedure |
Weight | Weigh using baby scales or stand-on scales |
Length or height | Measure length with a measuring board or height with a stadiometer |
Head circumference | Measure using non-stretchable (paper) tape measure < 2 years |
Fontanelle | Palpate anterior and posterior fontanelles |
BMI | See 1.7 Calculating BMI |
- Weighing children < 2 years of age 1
- Ensure the baby scales are accurate and regularly calibrated
- Bare weigh all babies to 2 years of age
- Zero the scales if required
- Record the weight to the nearest gram (g)
- Weighing children > 2 years of age 1
- Ensure the stand-on or chair scales are accurate and regularly calibrated
- Ensure the child removes all heavy clothing, shoes, jumpers etc.
- Zero scales if required
- Position the child on the centre of the scales so body weight is distributed evenly
- Record the weight to the nearest gram (g)
- Measuring length < 2 years of age 1
- For accuracy, this measurement requires 2 people; clinician and parent
- Flexible plastic measuring boards are less accurate, but good for home visiting
- Remove shoes and any excessive clothing
- Lay baby on their back (supine) on the measuring board
- Ask parent to hold the top of the baby’s head (crown) against the headboard by placing their hands either side of the baby’s head
- Inform parent that you will extend the baby’s legs while they ensure the crown stays against the headboard
- Ensure the shoulders and buttocks are flat against the measuring board
- Extend both the baby’s legs at the hips, keeping the back of the knees flat against the board by adding a slight amount of traction (pull)
- Slide the foot plate level with the base of both the baby’s feet
- The length is recorded to the nearest millimetre (mm)
- Measuring height > 2 years of age 1
- Ensure the stadiometer is accurate
- Remove child’s shoes
- Position the child with their head, back, buttocks and heels against the wall
- Ask them to stand straight with weight distributed evenly, heels together, looking forward and arms hanging by their sides
- Pull the measuring plate down to the top of their scalp
- Record the measurement to the nearest millimetre (mm)
- Measuring head circumference < 2 years of age 1
- Use a non-stretchable (paper) tape measure
- Position the child laying down, sitting up or in the parent’s arms
- Remove any objects from the child’s hair
- Identify the broadest section of the child’s skull
- Place the measuring tape slightly above the eyebrows and pinna of the ears and around the occipital prominence at the back of the skull
- Measure to nearest millimetre (mm)
- Repeat measurement
- If the two measurements differ by more than 3 mm take a third measurement
- Record the average of the 2 largest measurements
- Palpating fontanelles < 18 months of age 1
- Sit or lay the child on examination table or have the parent hold them in their arms
- Gently palpate the anterior (front) and posterior (rear) fontanelles for openness, size, or whether bulging or depressed
- Calculating BMI 1–3
- Calculate BMI using the below calculation OR plot weight-to-height on an age appropriate BMI chart OR use an online calculator. See Resource 2.
BMI = weight in kilograms (kgs) ÷ height in metres squared (m2
- Calculating BMI in children > 10 years is important to identify risk of chronic conditions early
2. Results
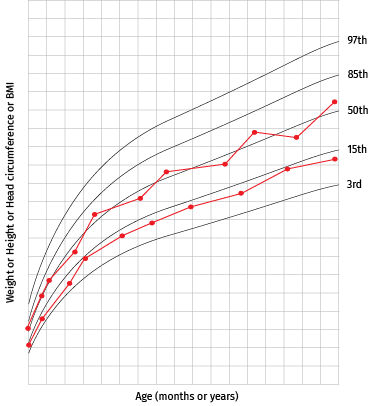
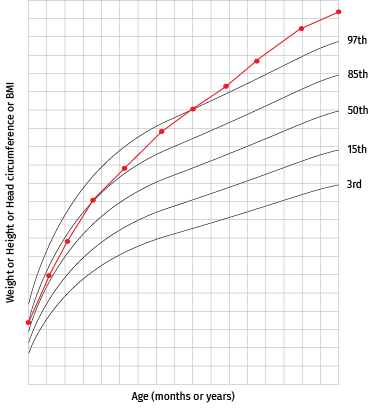
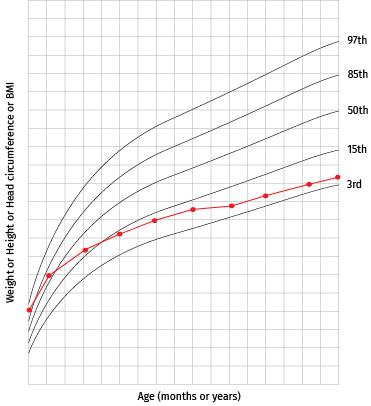
- Interpretation 1
- View the current plotted result in relation to past plotted results
- For clearer interpretation plotted points should be joined to form a continuous line and note:
- how the line tracks and moves in relation to the surrounding centile lines
- multiple plotted points over a short time will produce a jagged line
- few plotted points over a longer time produces long smoother lines
- A healthy child’s measurement should generally, over time, follow a consistent curve in relation to surrounding centile lines
- Weight gain for children to 12 months 1,2
- A general guide for weight gain variation is:
- an initial weight loss (up to 10% of the birth weight) after birth
- weight gains by 4–6 days of age
- return to birth weight by 2 weeks of age
- gains of 150–200 g/week up to 3 months
- from 3 months of age children should consistently gain weight over time, tracking along their centile line
- A general guide for weight gain variation is:
- Head circumference and length 1
- Head circumference should consistently increase over time, tracking along their centile line
- Children’s fontanelles 1
- For infants < 6 months of age, the anterior fontanelle diameter generally does not exceed 4–5 cm, should feel soft and slightly depressed with some pulsation
- In a markedly depressed fontanelle the cranial bones around the edge of the fontanelle can be easily palpated and visualised. This indicates dehydration
- A bulging fontanelle feels tense with marked pulsations, and may indicate an episode of prolonged crying or increased intracranial pressure from infection
- The fontanelles should get progressively smaller beyond 6 months of age
- The anterior fontanelle closes by 18 months of age and posterior by 2 months
- BMI for children 1–3
- BMI categories for children are:
- < 5th centile–underweight
- 25th to < 84th centile–healthy weight
- 85th to < 94th centile–overweight
- > 95th centile–obese
- A child > 10 years of age with a BMI > 85th centile risks developing chronic conditions.See Special considerations (child)
- BMI categories for children are:
Figure 1. Growth chart interpretation | |
|---|---|
Normal ideal
|
|
Abnormal
Possible causes
|
|
Abnormal
Possible causes
|
|
3. Brief intervention 1–3
- Reassure parents that a child tracking along a centile is normal, even if the centile is low (i.e. 3rd %ile)
- Provide Diet and nutrition and Physical activity and sleep related Resources 4. to parents of children with low or high weight or BMI measurements
- Children > 10 years of age with a BMI > 85th centile will require frequent pathology investigations. See Special considerations (child). Discuss the association of an elevated BMI with:
- adult obesity
- type 2 diabetes
- hypertension
- stroke
- heart disease
- depression
4. Referral
- For a bulging or depressed fontanelle refer to the Primary Clinical Care Manual
- Refer to a MO/NP, child health nurse or dietitian for further investigations if the child’s:
- measurements indicate rapid growth or decline
- different body measurements vary by 2 or more centiles when compared with one another e.g. weight on the 10th centile and length on the 75th centile
- if a child’s fontanelles are too wide, close early or remain open longer than expected for age
- If child’s weight measurements have crossed 2 centiles in an upward trajectory or is > 97th centile manage as per Overweight and obesity (child)
- If child’s weight measurements have crossed 2 centiles in a downward trajectory manage as per Poor growth (child)
- If a child > 10 years has a BMI > 85th centile manage as per Special considerations (child)
5. Follow-up
- Place the child on a recall register to monitor growth if required
- Ensure all referrals are actioned
- Provide the parent with details for the next scheduled follow-up appointment
6. References
- All Chronic Conditions Manual references are available via the downloadable References PDF